Genetic Causes of Recurrent Pregnancy Loss: Insights into Diagnosis and Future Directions
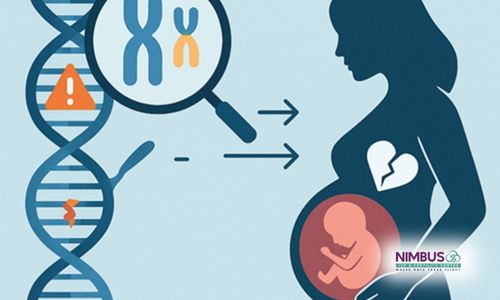
Recurrent pregnancy loss (RPL) is a distressing condition affecting approximately 1-2% of couples attempting to conceive. While multiple factors contribute to RPL, genetic and epigenetic abnormalities play a significant role. Understanding these underlying causes can help guide clinical management and improve reproductive outcomes.
Genetic and Epigenetic Causes of Recurrent Pregnancy Loss
- Chromosomal Abnormalities
Chromosomal abnormalities are one of the most common genetic causes of RPL, occurring in about 50-60% of cases of early miscarriage. These abnormalities can be classified as follows:
- Numerical Chromosomal Abnormalities (Aneuploidies)
- Trisomies: Extra copies of a chromosome, such as Trisomy 16, are frequently observed in spontaneous miscarriages.
- Monosomy X (Turner Syndrome): A missing X chromosome is one of the most common chromosomal causes of early pregnancy loss.
- Polyploidy: Triploidy and tetraploidy contribute significantly to early miscarriages.
- Structural Chromosomal Abnormalities
- Balanced Translocations: In approximately 3-5% of RPL cases, one partner carries a balanced reciprocal or Robertsonian translocation, leading to unbalanced chromosomal segregation in the embryo.
- Inversions and Deletions: Structural rearrangements like pericentric inversions and microdeletions can lead to implantation failure and pregnancy loss.
- Single-Gene Disorders
Although less common than chromosomal abnormalities, monogenic disorders can contribute to RPL, especially in consanguineous couples or those with a family history of genetic disorders.
- Autosomal Dominant Disorders: Conditions like Marfan syndrome or autosomal-dominant polycystic kidney disease (ADPKD) can increase the risk of pregnancy complications.
- Autosomal Recessive Disorders: Rare genetic disorders, such as congenital adrenal hyperplasia, may lead to recurrent pregnancy loss.
- Thrombophilia-Associated Mutations: Mutations in genes like F5 (Factor V Leiden), F2 (prothrombin G20210A), and MTHFR have been implicated in RPL due to increased risk of thrombosis and placental insufficiency.
- Epigenetic Factors
Epigenetic modifications, including DNA methylation and histone modifications, influence gene expression without altering the DNA sequence. Aberrant epigenetic regulation has been associated with implantation failure and pregnancy loss.
- Parental Imprinting Disorders: Abnormal methylation patterns in genes such as H19/IGF2 can lead to pregnancy loss.
- Advanced Maternal Age: Aging affects DNA methylation, which can contribute to embryonic developmental defects.
- Environmental Factors: Exposure to toxins, smoking, or endocrine disruptors can induce epigenetic changes, increasing miscarriage risk.
Genetic Testing and Diagnostic Approaches
To identify genetic causes of RPL, various genetic tests are available:
- Karyotyping: Standard cytogenetic analysis of parents and products of conception (POC) helps identify translocations and aneuploidies.
- Chromosomal Microarray (CMA): Detects submicroscopic chromosomal deletions or duplications not visible on karyotyping.
- Next-Generation Sequencing (NGS): Allows for the identification of single-gene mutations and rare genetic variants.
- Preimplantation Genetic Testing (PGT): Used in in vitro fertilization (IVF) to screen embryos for chromosomal abnormalities before implantation.
- Whole-Exome Sequencing (WES): Identifies novel monogenic disorders associated with pregnancy loss.
Treatment Strategies
Based on the identified genetic cause, treatment options can be tailored to improve pregnancy outcomes:
- Assisted Reproductive Technologies (ART): IVF combined with PGT can help select genetically normal embryos for implantation.
- Anticoagulation Therapy: For individuals with thrombophilia-related mutations, anticoagulants such as low-molecular-weight heparin (LMWH) and aspirin are used.
- Hormonal and Immunomodulatory Therapies: Progesterone supplementation and intravenous immunoglobulin (IVIG) may benefit selected cases with epigenetic dysregulation.
- Gene Therapy and Epigenetic Modulators: Although still in experimental stages, future treatments may target specific genetic mutations and epigenetic alterations to reduce miscarriage risk.
Emerging Research and Future Directions
With advancements in reproductive genetics, researchers are exploring new frontiers in understanding and treating RPL:
- Multi-Omics Approaches: Integrating genomics, transcriptomics, and epigenomics to uncover novel biomarkers.
- CRISPR-Based Gene Editing: Potentially correcting genetic mutations in embryos.
- Artificial Intelligence in Reproductive Medicine: AI-based models are being developed to predict miscarriage risk based on genetic and clinical data.
Genetic and epigenetic factors contribute significantly to recurrent pregnancy loss. Advances in genetic diagnostics and personalized treatment strategies provide hope for affected couples. Continued research into the genetic underpinnings of RPL will pave the way for improved reproductive success and tailored therapeutic interventions